Prolapse
One woman out of 3 over 50 years old has a prolapse, often minor and symptomless. However, prolapses worsen and become symptomatic, especially pass 60 years old.
Women describe a vaginal ball, a sensation of something going down or/and of heaviness. Before to explain what a prolapse is, it is essential to understand how the concerning organs sit inside our abdomen.
A bit of anatomy!
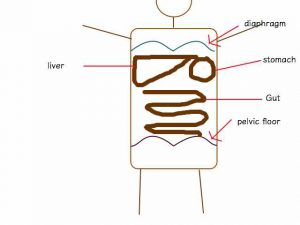
Your abdomen is like a tube with your abdominal muscles in front, the vertebral spine at the back, diaphragm on top like a roof and pelvic floor muscles at the bottom (like a floor!). This tube is very malleable and can change is shape (bend forward/backward, on the side, etc…). However, a lot of these movements increase your intra-abdominal pressure. Consequently, one of the mains purposes of the abdominal and pelvic floor muscles is to resist these pressures to keep everything together!
In the abdominal space everything moves!
All day long our bladder and rectum are filled and emptied, changing their shapes and moving their surroundings.
Your uterus also follows their movements and gets filled and emptied throughout menstrual cycle and pregnancy…
Similarly, each breath, filling your lungs, changes the shape and pressure of your abdomen.
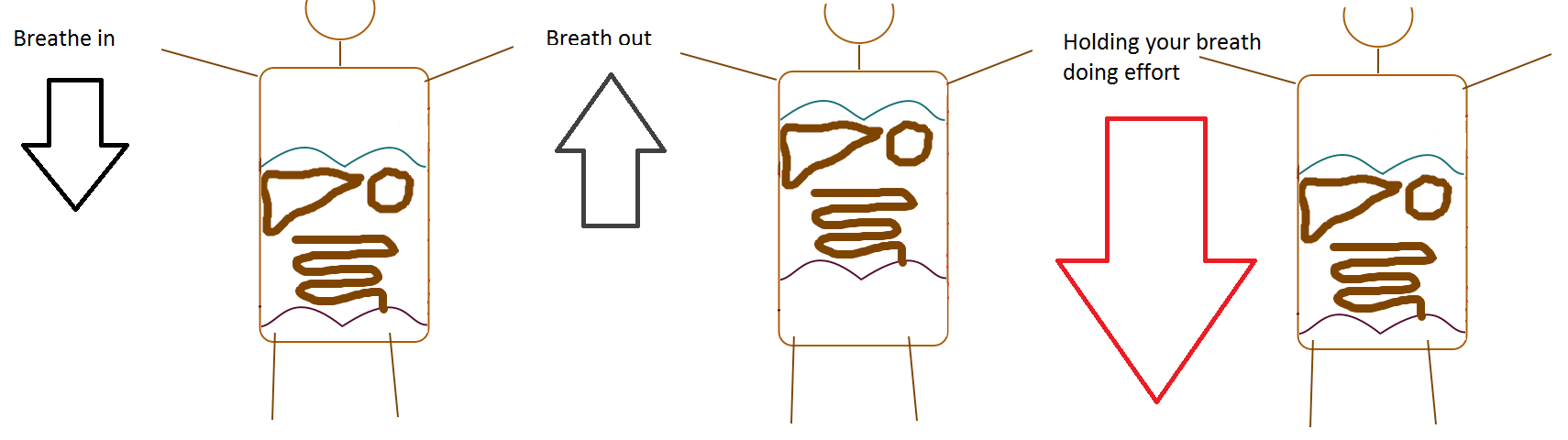
As we breathe in, diaphragm lower increasing intra-abdominal pressure, pushing your visceral organs and pelvic floor downward and, your abdominal muscles forward (thus the sensation of inflating belly).
Whereas as we breathe out, diaphragm rises, bringing abdominal organs and pelvic floor upward. It also brings abdominal muscles inward creating a “flat belly”.
Therefore, if you perform an effort (like lifting, pushing, carrying…) during a blocked inhalation (holding your breath just after breathing in), you already have your abdominal organ and pelvic floor in a low position but you push them downward even more as you produce your effort.
Furthermore, each abdominal organ is held by ligaments, which get weaker over the years and are strongly influence by your hormones (relaxing/weakening during pregnancy and menopause).
This weakening phenomenon and the constant downward push (gravity and diaphragm) may lead to organs fall. For woman, the risk is majored by the “gap” between the bladder and rectum: the vagina.
What is a prolapse? How is it defined?
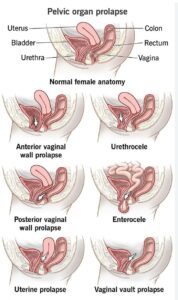
We speak about genital-urinary prolapse when there is a temporary or permanent lowering of one or more pelvic organs. They will push and deform the vaginal wall, creating a bump on the perineum or even exiting through the vagina.
These pelvic organs are:
- Bladder: named cystocele
- Uterus: named hysterocele
- More rarely Rectum: named rectocele
What are prolapse risks factors?
As I explain previously prolapses can be caused by
- Hormonal changes, such as in pregnancy or menopause, which weaken support ligaments holding pelvic organs
- Obstetrical trauma, like a delivery which is a violent and prolong downward push, stretching support ligaments and muscles
- Surgery, for example hysterectomy
- Repetitive increase of intra-abdominal pressure, like in certain sports, bad abdominal exercises (sit up, crunches, one hundred…), chronic cough, constipation…
- Important and rapid weight gain
How to treat a prolapse?
1) Surgery : the prolapse cure
What is the aim of prolapse surgery?
It aims to put back the prolapsed organ to its initial position and to fix it there.
How do they perform prolapse surgery?
There are two main possibilities abdominal or vaginal:
a) Abdominal
Surgeon performs a horizontal opening between pubis and belly button. Prolapsed organ is fixed to a solid element.
b) Vaginal
In this case, prolapse surgery is performed through natural pathway. With this method, for bladder and uterine prolapses no incisions are needed. However, rectocele prolapse still require an incision. The aim is the same as for abdominal approach; fix the prolapse organ to a solid element.
Prolapse surgeries can be associated to a surgery for effort incontinence. A string is passed under the urethral canal which brings urine from the bladder to the vulva.
What are the risks of prolapse surgery?
This surgery is now more or less common with few risks.
However, in addition to risks associate to any surgery (infection), the main risks are absence of improvement of effort incontinence, residual prolapse or even apparition of a discomfort during sexual intercourse.
Sometimes, even after an initially successful, a prolapses or urinary incontinence may reappear if the initial causes of the prolapses were not treated, such as constipation, pelvic floor and abdominal transverse muscles weakness, hyperperssive effort (as describe above with breathing mechanism), bad abdominal exercises (crunches, sit up, one hundred) or even some sports with repetitive impact.
2) Prolapse Rehabilitation
 It aims to prevent or to slow down the developing prolapse by identifying causing and aggravating factors. Also, it helps to diminish symptoms linked to prolapse (discomfort, incontinence…). Finally, in more advance stage, it prepares surgery and improves its outcomes by preventing secondary incontinence and prolapse reoccurrence.
It aims to prevent or to slow down the developing prolapse by identifying causing and aggravating factors. Also, it helps to diminish symptoms linked to prolapse (discomfort, incontinence…). Finally, in more advance stage, it prepares surgery and improves its outcomes by preventing secondary incontinence and prolapse reoccurrence.
Prolapse rehabilitation is multi-factorial and global as various factors cause prolapses: pelvic floor competence (its tonicity, ability to contract/control muscles, its automatization in effort…), abdominal competence (its ability to control and orientate pressure created in physical activities), effort management, diaphragm function and lumbar/pelvic static.
To learn more about prolapse rehabilitation, have a look at pelvic floor rehabilitation and zero pressure gymnastic.
3) Pessary
What is it?
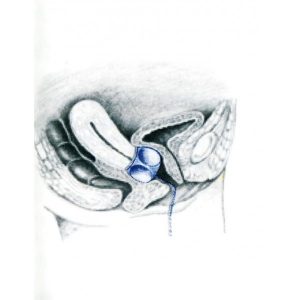 Pessary is a silicone cube placed intra-vaginally to avoid prolapse aggravation and to diminish related symptoms (heaviness, pain, hollowness, effort incontinence)
Pessary is a silicone cube placed intra-vaginally to avoid prolapse aggravation and to diminish related symptoms (heaviness, pain, hollowness, effort incontinence)
How does pessary work?
It comes underneath the prolapse organ to compensate muscle and ligament weakness.
Consequently, it doesn’t cure prolapse but helps to maintain a “normal life” despite the prolapse avoiding surgery solution.
How to use a pessary?
Always ask to your gynaecologist or women health physiotherapist. He or she will check the correct pessary size and will teach you how to put it. It is easy, but always beneficial to have professional advices before to manage it on your own! Pessary requires use of lubricant and sometimes of an oestrogen cream in case of menopausal symptoms.