
From one country to another, pregnancy monitoring can vary drastically, from the number of ultrasound checks to how the due date is calculated!
Unfortunately, the quality of care is not always as good as in France and language can often be a barrier to good communication with health care staff. However, don’t panic, through this article, we will see how to be ready to give birth in good condition, no matter where you are on the globe!
Anatomy of perineum and pelvis
It is already essential to understand your body and how it is formed in order to prepare for childbirth. Let’s do a little anatomical reminder.
Pelvis : The body unit containing the viscera.
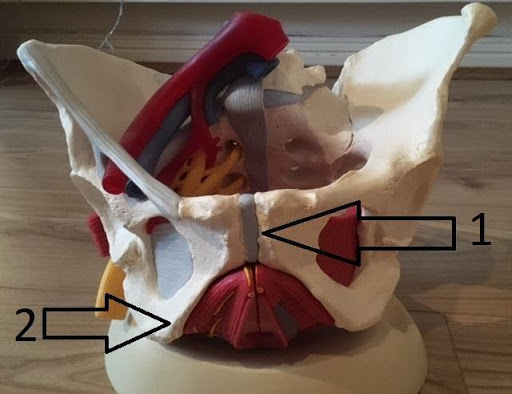
#1 The pubic symphysis is the bone that can become “disjointed” during pregnancy, creating pain in the crotch or along the adductors.
#2: The ischiums are the bones in the buttocks that you sit on. During pregnancy, this area is often painful due to contractures of the piriformis muscle (here is a video on how to stretch them)
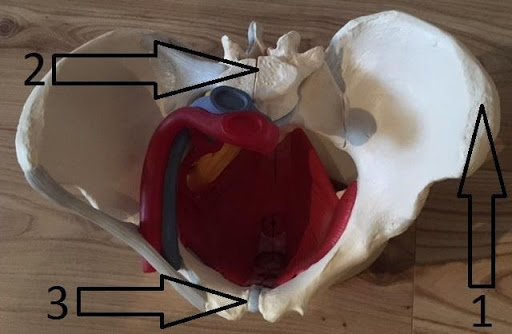
#1: The iliac crests are the relief felt on the side of the lower abdomen and end in a point that is felt at the top of the legs.
#2: vertebrae
#3: pubic syphysis
Genitalia
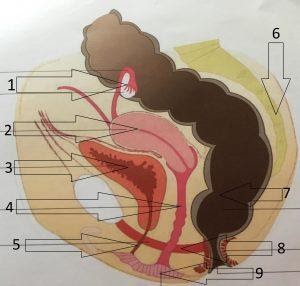
#1 Ovary
#2 Uterus suspended and attached to the sacrum by the uterine ligaments
#3 The bladder rests on the symphysis pubis
#4The vagina is a large void in the middle of this enclosure
#5 The urethra is the channel through which the bladder is emptied
#6 Sacrum
#7 The rectum and anal canal (anus) are connected by an angle that prevents the passage of stool from the rectum into the anal canal (to maintain continence)
#8 Perineal muscles
#9 Vagina
Pelvic Floor
The pelvic floor is a kind of inverted hammock that provides balance and support for the pelvic viscera.
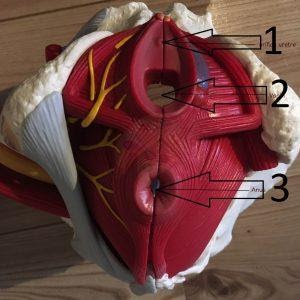
- #1 Urethral orifices
- #2 Vagina
- #3 Anus
If you want to know more about the anatomy of the pelvis and the perineum you can read our article or watch our Youtube video on this subject:
Understanding childbirth
What is the date term ?
In France, it is considered that you give birth at 41 weeks of amenorrhea (39 weeks of pregnancy). This is not the same everywhere! In England, for example, it is 39 weeks. In any case, your baby will be considered premature if it arrives before 37 weeks of amenorrhea and very premature before 32 weeks of amenorrhea. After 41 weeks of amenorrhoea, the baby is said to be overdue. You should seek immediate advice, as this can be dangerous for your baby and yourself
What are the stages of childbirth ?
Stage 1 . the working stage
You feel the first regular contractions (usually every hour at first) and your cervix starts to change, to dilate. Sometimes there may be contractions without any changes to the cervix, a kind of “false labour”, this is not serious but not yet the time to go to hospital (although let’s be honest, you will only realise this when the midwife checks your cervix and tells you to go home as it is too early!) Then these contractions will increase in frequency, intensity and duration. The water will either break naturally or the midwife will break the membranes. Your baby can be in 3 different positions:
- Cephalic: This is the most common. The baby has its head down, ready to come out! You can prepare for a vaginal delivery (if there are no other problems of course!)
- Breech: The baby’s bottom is down, sitting on your perineum so to speak. Unfortunately, in this position, the obstetrician will suggest a caesarean section in most cases.
- Transverse: Your baby is lying in the womb with the head on the right and the feet on the left or vice versa. This is also an indication for a Caesarean section.
Stage 2 : Engaging stage
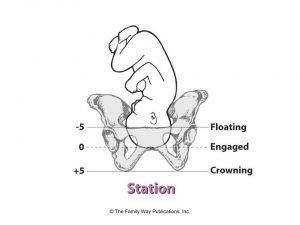
Thanks to the uterine contractions, your baby descends and engages its head in the upper part of the pelvis. You start to feel the pressure of his head on your perineum and a pushing sensation on your rectum. You feel like it’s time to start pushing, and you’re right! There are some positions that can help your baby to descend.
We list several positions for uterine contractions in this video, down here :
Stage 3 :Expulsion stage
Normally this phase lasts about thirty minutes. But sometimes it can last much longer, which is why the pelvis and perineum are not damaged in the same way from one delivery to another. It is just before this phase that the obstetrician may choose to use a catheter to empty your bladder if it is full.
To summarise:
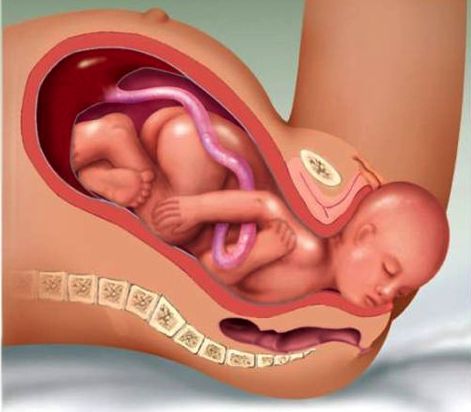
Your baby enters the upper part of the pelvis and then turns its head to face the sacrum (the bone in the lower back) to descend into the lower part of the pelvis.
The top of the baby’s head touches the lower part of the pubic symphysis (the bone between the legs) and can come down through the posterior perineum muscle.
Each contraction will allow the baby to descend more and more.
For this stage, breathing is very important. Good breathing techniques will allow you to push more efficiently to help your baby come out but also to avoid creating too much pressure and therefore less damage to your perineum!
Stage 4 : Baby expulsion
The baby’s neck rests on the pubic symphysis, the head is deflected to come out. When the baby is out, the midwife accompanies the child to free the shoulders and to take out the rest of the body.
Stage 5 : Delivery of the baby
Your baby is giving its first cry and the midwife is holding it in her arms. You might think it’s over, but it’s not!
30 minutes after the baby has been expelled, the placenta must now be expelled. If the placenta does not come out naturally, the midwife will have to perform a manoeuvre to remove it by placing her hand in the uterus. This is quite painful but essential to avoid infection or sepsis. It is normal to lose 500ml of blood during childbirth. If you lose more than 500ml, it is called a haemorrhage and you will need a transfusion. This is very common but it (among other things!) explains why you feel exhausted after giving birth.
Complementary techniques
This generic term includes epidural, episiotomy and instrumental extractions (forceps and vacuum). All of these techniques are highly controversial and their use varies greatly from country to country. We are not going to go into detail here, as each one deserves its own article to explain them and especially to explain the pros and cons!
So there you have it!
you know pretty much everything that can happen to you during childbirth. Remember to do your perineum exercises (contraction and relaxation), breathing exercises and pelvic exercises to make your delivery easier and avoid complications. If you don’t know how to do this, please watch our video on the subject!



