The aim of rehabilitation is not only to treat the initial cause of the injury but also to reduce and prevent compensations and their negative effects.
Most orthopedic rehabilitations after trauma or surgery follow the same steps:
The difference in duration of each of these stages will vary depending on the initial injury, patient goals, and time spent in self-exercise.
At My French Physio, we offer treatments adapted to the elderly, especially rehabilitation sessions after an operation.
Pathologies
Treatments

During abdominal surgery (caesarean section, removal of appendicitis), the surgeon cuts various layers from the skin to the organs, including the muscles and fascia.
During healing, these sheets close completely but unfortunately sometimes create scar tissue.
These adhesions are troublesome because they prevent the movement and normal function of the different tissues.
For example, an adhesion between muscle and organ will decrease the capacity for muscle contraction, creating weakness or even pain.
Thanks to visceral osteopathy, the therapist will not only improve the elasticity of the poorly mobile areas of your abdomen, but he will also use a global approach to analyze how this abdominal dysfunction impacts the rest of the body with a particular interest in the diaphragm and clearing postures.
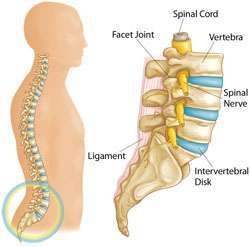 lumbar spine elements
lumbar spine elements
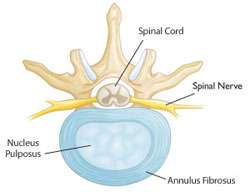 Annulus fibrosus : It is the hard and flexible periphery of the disc
Nucleus pulposus is the central part that is soft like jelly (but containing tens of thousands of cells).
Annulus fibrosus : It is the hard and flexible periphery of the disc
Nucleus pulposus is the central part that is soft like jelly (but containing tens of thousands of cells).
If you tear the anterior cruciate ligament (ACL) in your knee, you may need to have reconstructive surgery.
The ACL is a tough band of tissue that connects the thigh bone to the tibia bone at the knee joint.
It extends diagonally inside the knee and gives the knee joint its stability. It also helps control the back and forth movement of the lower leg.
ACL injuries
Knee injuries can occur when playing sports such as skiing, tennis, squash, football and rugby. ACL injuries are one of the most common types of knee injuries, accounting for about 40% of all sports injuries.
You can tear your ACL if your lower leg extends too far forward. It can also tear if your knee and lower leg are twisted.
The most common causes of an ACL injury are:
a bad landing during a jump
suddenly stopping
change direction suddenly
having a collision, for example during a football tackle
If the ACL is torn, your knee can become very unstable and lose its full range of motion.
This can make it difficult to perform certain movements, such as turning in place. Some sports may be impossible to play.
What are menisci?
Menisci are C-shaped tissues inside the knee joint, located between the cartilaginous surfaces of the thigh (femoral) and tibia (tibia). Both are found in the joint. There is one on the inside of the knee (medial) and another on the outside (lateral). The outer parts have sufficient blood supply, but the middle and inner parts have insufficient blood supply. As the blood supply can affect healing, the location of a tear will affect treatment options.
What are the functions of the meniscus?
Menisci are tissues that respond to force and load. They have several important functions: increasing the stability of the knee joint, lubricating the joint, helping balance, absorbing shocks, transmitting the load (more even distribution of weight and stress on the joint knee).
What are the types of meniscal lesions?
The menisci are among the most commonly injured parts of the knee joint. There are different types of meniscal injuries: – acute meniscal tears (due to a specific injury) – degenerative meniscal tears (not due to a specific injury). It is important to know the difference between these two types of injuries because the way we treat them is different.
A dislocated patella (or kneecap) is a common injury that normally takes about 6 weeks to heal.
It is often caused by a sudden knock or change in direction when the leg is placed on the ground, for example during sports or dancing.
The patella is normally located on the front of the knee. It slides over a groove in the joint as you bend or straighten your leg.
When the kneecap dislocates, it comes out of this groove and the supporting tissues can be stretched or torn.
Symptoms of a dislocated kneecap
When a kneecap dislocates, it usually looks misplaced or at an odd angle. But in many cases, it snaps back into place soon after.
Other symptoms include
a “pop” feeling.
severe knee pain
being unable to straighten the knee
sudden swelling of the knee
being unable to walk
Knee replacement surgery (arthroplasty) is a common operation that involves replacing a damaged, worn or diseased knee with an artificial joint.
Adults of any age can be considered for knee replacement surgery, although most operations are done on people between the ages of 60 and 80.
A smaller operation, called a partial knee replacement, is usually done on younger people, between 55 and 64 years old, where the artificial joint should have to be redone within ten years.
A tibial plateau fracture is a fracture of the upper part of the tibia (tibia-barred) that involves the knee joint. Symptoms include pain, swelling, and a decreased ability to move the knee. People are generally unable to walk. Complication can include artery or nerve injury, arthritis, and compartment syndrome.
The cause is usually trauma, such as a fall or collision with a motor vehicle. Risk factors include osteoporosis and certain sports such as skiing. The diagnosis is usually suspected based on symptoms and confirmed by x-rays and a CT scan. Some fractures may not be visible on a simple x-ray.
Pain can be managed with NSAIDs, opioids, and a splint. In people who are otherwise healthy, treatment is usually done by surgery. Sometimes, if the bones are properly aligned and the ligaments in the knee are intact, people can be treated without surgery.
They account for about 1% of fractures and most often occur in middle-aged men and older women [3]. In the 1920s, they were called “wing fractures” because of their association with people struck by a motor vehicle while walking.
Hip fractures are cracks or breaks in the upper part of the thigh bone (femur) near the hip joint. They are usually caused by a fall or injury to the side of the hip, but sometimes can be due to a health problem, such as cancer that weakens the hip bone.
Falls are very common in older people, especially those over 80, who may have reduced vision or problems with mobility and balance.
Hip fractures are also more common in women, who are more likely to have osteoporosis, a disease that makes bones weak and brittle.
Symptoms of a hip fracture
Symptoms of a hip fracture after a fall may include
A hip fracture does not necessarily cause bruising or prevent you from standing or walking.
Hip replacement surgery is a common type of surgery that replaces a damaged hip joint with an artificial joint (called an implant).
Adults of any age can be considered for a hip replacement, although most operations are performed on people aged 60 to 80.
A modern artificial hip joint is designed to last at least 15 years. Most people have a significant reduction in pain and an improvement in their range of motion.
When a hip prosthesis is needed
Hip replacement surgery is usually needed when the hip joint is worn or damaged, so your mobility is reduced and you are in pain even while at rest.
The most common reason for hip replacement surgery is osteoarthritis. Other conditions can cause damage to the hip joint:
rheumatoid arthritis
hip fracture
septic arthritis
disorders that cause unusual bone growth (bone dysplasias)
This intervention is mainly performed in the event of bone loss of the anterior surface of the glenoid (following a bone lesion of the bankart type or repeated dislocations which wear out the anterior surface of the glenoid).
It was first described by a French surgeon, Michel Latarjet, in 1954. Similar procedures have also been used, such as the Bristow procedure in the UK and the Boytchev procedure in Russia. However, the Latarjet procedure has become the most popular globally due to its low recurrence rate and excellent published results.
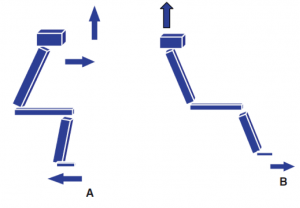
The procedure involves the transfer of the coracoid with its muscles attached to the deficient area on the front of the glenoid. This replaces the missing bone and the transferred muscle also acts as additional muscle support preventing further dislocations. The procedure has a high success rate (recurrence rate less than 1% 4) and this is due to the “triple effect” described by Patte. These are 1) increase or restore the contact surface of the glenoid; 2) the joint tendon stabilizes the joint when the arm is in abduction and external rotation,
Shoulder replacement is a surgical procedure to treat the shoulder joint if it has been damaged or worn out, usually from arthritis or injury. Your surgeon replaces part or all of your shoulder joint with artificial parts.
Your shoulder is a ball joint. The ball at the top of your arm moves smoothly into the cavity of your shoulder blade on a lining of cartilage. Cartilage prevents your bones from rubbing against each other. If your cartilage is damaged by injury or arthritis, it can make your joint painful and stiff.
A new shoulder joint can help improve shoulder movement and reduce pain in the shoulder. Artificial parts of the shoulder are usually made of metal or plastic or a combination of these materials.
The average age of people who have a shoulder replacement is around 70, and many people are well over that age. An artificial shoulder joint usually lasts at least 10 years, often much longer.
Types of shoulder prostheses
There are several types of shoulder replacement. Your surgeon will discuss with you the best procedure for your particular case. This will depend on the condition of the muscles around your shoulder, the stability of your shoulder, and the strength of your bones.
The three main types of shoulder replacement procedure are described here.
Reverse shoulder replacement
This is the most commonly used shoulder replacement procedure. It gets its name from the fact that the positions of the kneecap in your joint are reversed. A metal ball is attached to your shoulder blade, where your socket used to be. And a new cavity is attached to the top of your arm, where the ball was previously. The new ball and the new cavity each have a rod which, together with a special cement, helps to anchor them to your bone.
Total shoulder replacement
The second most common type of procedure is total shoulder arthroplasty. If you have this type of operation, your surgeon will replace the ball at the top of your arm with a new metal ball. It will also replace your shoulder blade cavity with a new cavity. These replacements mimic the original structure of your shoulder.
Partial shoulder replacement (hemiarthroplasty)
In the case of a partial shoulder replacement, only the ball located at the top of the arm is replaced. The new metal ball will then move into your existing cavity.
Fractures of the proximal humerus are common and account for 5% of all fractures. These fractures tend to occur in elderly patients who are osteoporotic.
The most common mechanism for these fractures is a fall onto the outstretched hand from a standing height. In younger patients, high energy trauma is the cause of the injury.
The goal of treating fractures of the proximal humerus is to allow bone and soft tissue to heal in a normal anatomical position in order to maximize upper limb function.
Most fractures are minimally displaced and stable, so surgical fixation is not necessary. A supportive sling followed by early rehabilitation and have good functional results.
Displaced fractures require reconstruction, because if left untreated they are likely to produce limited function.
The most common definition of displacement is 1 cm between fragments or 45 ° of angulation between fragments of the fracture. The parts that most often produce these fragments are the humeral head, the upper and lower tuberosities, and the surgical neck.
A broken ankle usually takes 6 to 8 weeks to heal, but it can take longer.
The doctor will tell you:
How long you will need to wear the boot or have a cast, how much weight to put on your ankle, you may be given crutches or a walker to help keep weight off.
Once healed, use your ankle as if it were normal. By moving it, you will prevent it from stiffening.
You may need to see a physical therapist. It can help you do exercises to get your foot and ankle moving smoothly again.
Ask your doctor when you can resume contact sports or other activities that place a heavy strain on your ankle.
What are the ankle ligaments?
The ankle is a hinged joint between the leg and the foot, which allows you to move up and down. The bones of the leg (tibia and fibula) form a slit, and the talus of the foot fits between them. The talus is held at the tibia and fibula by strong bands of tissue called ligaments. Each ligament is made up of many strands or fibers of a material called collagen, which is extremely strong.
The ligament inside the ankle (the deltoid ligament) is made up of two layers, the deeper being the more prominent. This ligament is mainly torn in association with severe fractures of the ankle bones. Sports injuries of this ligament are rare.
The ligament located on the outside of the ankle (lateral ligament) consists of three distinct bands: one in the front (anterior talofibular ligament), one in the middle (calcaneofibular ligament) and one at the rear ( posterior talofibular ligament). The anterior and central bands are the ligaments injured during a sprain.
TESTIMONIALS
Words of patients!
“Started with Mathilde at My French Physio 6 months ago after a knee operation. While always pushing me to work as hard as I can to recover, she is always very mindful of any pain or apprehension I might have. Mathilde has definitely played a very big part in my quick recovery! Nouria, the secretary, is also extremely nice and helpful for any queries I have. The team at My French Physio has definitely made my recovery a lot more fun than expected, would highly recommend!”
Pauline S.
“Elodie and Virgil have helped me and my children after both births for perineum physio and osteopathy. They form a strong team of professionals and are always very friendly. Their home visits are certainly a plus for mums. I cannot recommend them enough.”
Joana M.
“I have seen the team at My French Physio for the last 3-4 years after giving birth to my daughters and they are absolutely fantastic. Very professional, approachable and extremely good in their field, I can highly recommend them to anyone. Both Élodie and Virgil have helped me a lot!”
Valerie H.